Understanding Your Benefits for Vision Restoration Surgery
Vision restoration surgery has become an essential medical procedure for millions of Americans facing age-related vision impairment. As healthcare policies evolve and insurance frameworks adapt to changing medical standards, understanding how your benefits apply to necessary eye procedures is more important than ever. This comprehensive guide explores coverage options, eligibility requirements, and what patients should know when planning for vision restoration procedures in the coming years.
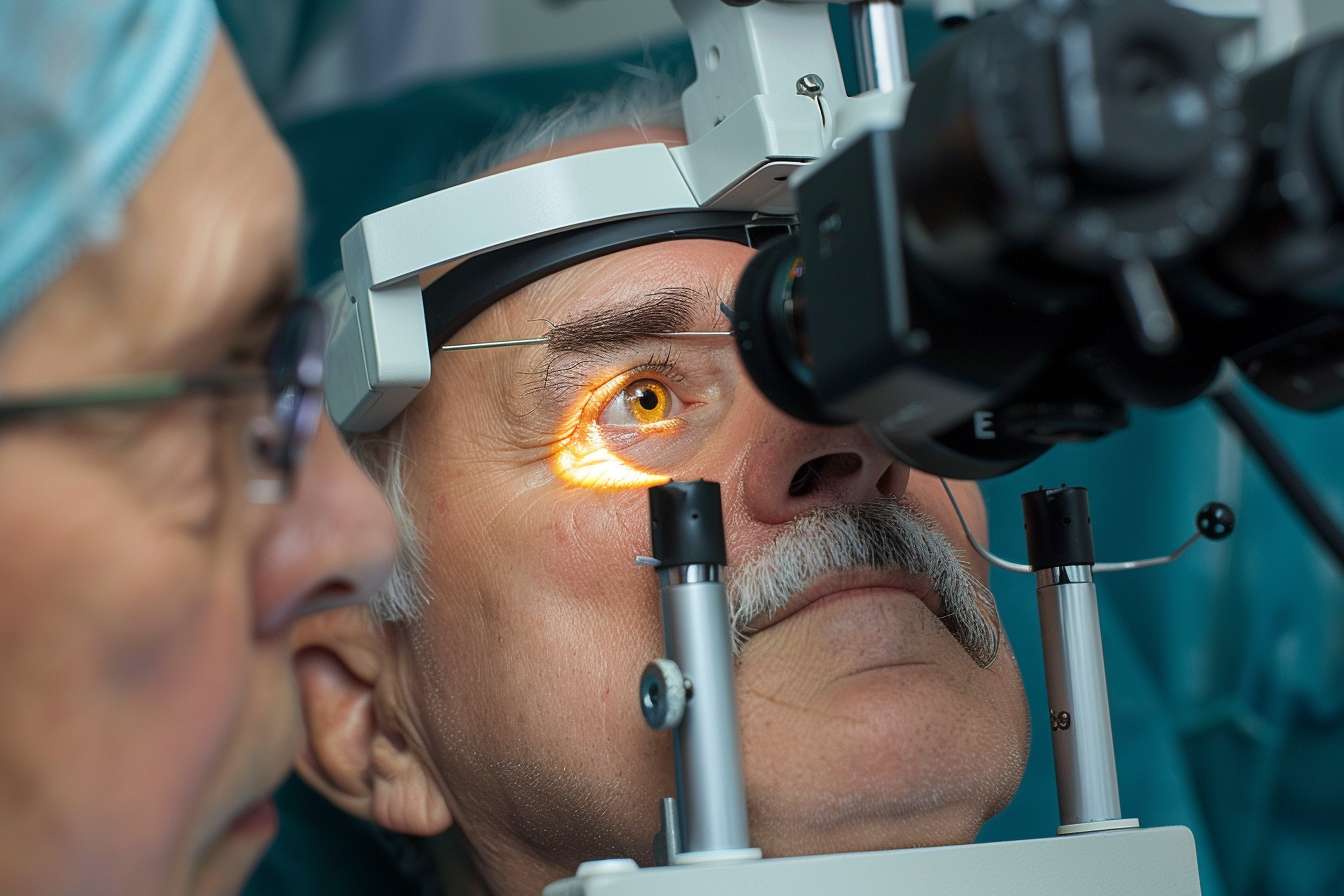
Vision impairment affects daily life in countless ways, from reading and driving to recognizing loved ones. For those experiencing clouding of the eye’s natural lens, surgical intervention often becomes medically necessary. Understanding how insurance benefits apply to these procedures helps patients make informed decisions about their eye health and financial planning.
Cataract Surgery Coverage in 2026
Insurance coverage for vision restoration procedures has evolved significantly over recent years. Most health insurance plans, including employer-sponsored coverage and government programs, recognize lens replacement surgery as a medically necessary procedure rather than an elective cosmetic treatment. Coverage typically includes the surgical procedure itself, pre-operative examinations, standard intraocular lens implants, and post-operative care. However, premium lens options that correct astigmatism or provide multifocal vision may require additional out-of-pocket expenses. Patients should review their specific plan documents to understand deductibles, copayments, and any coverage limitations that may apply to their situation.
Understanding Why Coverage Matters
The financial implications of vision restoration surgery extend beyond the procedure itself. Without adequate insurance coverage, patients face costs that can range from several thousand dollars per eye to significantly higher amounts depending on the facility, surgeon experience, and lens technology selected. Coverage matters because untreated vision impairment creates additional indirect costs through increased fall risks, reduced independence, and diminished quality of life. Insurance protection ensures that patients can access necessary medical care without facing financial hardship. Understanding your benefits helps you plan effectively, avoid unexpected expenses, and make informed choices about timing and treatment options. Many patients delay necessary procedures due to cost concerns, but comprehensive coverage can eliminate these barriers and enable timely intervention when vision impairment begins affecting daily activities.
Cost and Coverage Comparison
Understanding the financial landscape of vision restoration procedures helps patients plan effectively. The following comparison provides general estimates based on typical coverage scenarios:
| Coverage Type | Typical Patient Responsibility | Coverage Scope |
|---|---|---|
| Medicare Part B | 20% coinsurance after deductible | Medically necessary procedures, standard lenses, facility fees |
| Medicare Advantage | Varies by plan, often $0-$500 copay | Similar to Original Medicare, some plans offer enhanced benefits |
| Private Insurance | Deductible plus 10-30% coinsurance | Procedure, standard lenses, follow-up care |
| No Insurance | $3,000-$6,000 per eye | Full procedure cost, standard technology |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
How Insurance Providers Are Approaching 2026
Insurance companies continue refining their coverage policies for vision restoration procedures as medical technology advances and treatment protocols improve. Most major insurers maintain coverage for medically necessary lens replacement surgery while establishing clear guidelines about what qualifies as standard versus premium care. Many providers now require documented vision impairment that interferes with daily activities before approving coverage. Pre-authorization requirements have become more common, requiring patients and physicians to submit clinical documentation demonstrating medical necessity. Some insurance plans have expanded coverage to include advanced diagnostic testing and newer surgical techniques that improve outcomes. Provider networks also influence coverage, with in-network surgeons and facilities typically offering lower out-of-pocket costs. Patients should verify network participation before scheduling procedures to maximize their benefits and minimize unexpected expenses.
What Medicare Beneficiaries Should Expect
Medicare beneficiaries represent a significant portion of patients requiring vision restoration surgery, and understanding Medicare coverage specifics is essential for this population. Original Medicare Part B covers medically necessary lens replacement surgery performed in outpatient settings, including ambulatory surgical centers and hospital outpatient departments. Coverage includes one pair of standard eyeglasses or contact lenses following surgery. Beneficiaries typically pay 20 percent of the Medicare-approved amount after meeting their annual Part B deductible. Medicare Advantage plans must provide at least the same coverage as Original Medicare but may offer additional benefits such as routine vision care or allowances toward premium lens options. Medigap supplemental insurance can help cover the 20 percent coinsurance that Original Medicare does not pay. Beneficiaries should understand that while Medicare covers standard monofocal lenses, upgraded lenses that correct multiple vision issues may require additional payment, though the surgical procedure itself remains fully covered.
Planning for Your Procedure
Successful navigation of insurance benefits requires proactive planning and clear communication with healthcare providers and insurance representatives. Start by requesting a detailed explanation of benefits from your insurance company specifically addressing vision restoration procedures. Schedule a consultation with an ophthalmologist to assess your condition and obtain documentation of medical necessity. Ask your surgeon’s office about their experience working with your insurance plan and whether they can provide cost estimates based on your specific coverage. Verify that your chosen surgeon and surgical facility are in-network providers under your plan. Understand your plan’s pre-authorization requirements and ensure all necessary approvals are obtained before scheduling surgery. Review your annual deductible status and consider timing if you have other planned medical expenses. Finally, ask about payment plans or financing options if you anticipate out-of-pocket costs that exceed your immediate budget.
Understanding your insurance benefits for vision restoration surgery empowers you to make informed healthcare decisions without unnecessary financial stress. By thoroughly researching your coverage, communicating with providers, and planning ahead, you can focus on the most important outcome: restoring clear vision and improving your quality of life.




